Honoring America’s Allies
Good Shepherd Hospice, HPH Hospice and LifePath Hospice are each part of our veterans program. One way the hospice affiliates participate is by honoring veterans with a pinning ceremony. Each veteran is presented with a certificate to commemorate their sacrifice, along with a piece of an American flag that can be pinned to their shirt. Though this service is offered primarily to American veterans, any solider who served as an ally of the United States is eligible to be honored.
While the numbers are usually low, usually less than 10 foreign veterans are honored by each affiliate every year, it is important to pay tribute to all men and women who fought for and with the United States.
Stuart Peckham served in the Canadian Army alongside American soldiers
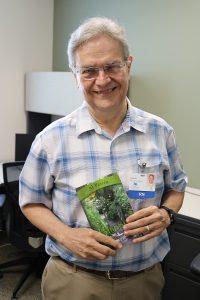
 Stuart Peckham, known as “Mr. P” to friends and family, is a patient with HPH Hospice. When he was 21 he served as a translator in the Highland Light Infantry 9th Brigade of the Canadian Army during World War II. He speaks three languages and landed at D-Day.
Stuart Peckham, known as “Mr. P” to friends and family, is a patient with HPH Hospice. When he was 21 he served as a translator in the Highland Light Infantry 9th Brigade of the Canadian Army during World War II. He speaks three languages and landed at D-Day.
“I left as a boy and came back as a man,” Mr. P said. “I had three brothers. We all served. We all came back.”
Born in 1924, as the son of Polish Jews, he lost 21 family members in the Holocaust. He was later adopted and raised Christian, but the war took him to some of the concentration camps where some of his relatives went and never returned.
Mr. P doesn’t like to talk about the war. He’d rather tell you about his careers in real estate, construction and as an auctioneer.
With a resume that impressive, it may not be surprising he’s also a writer.
He’s written 16 books, six even published, including one about the art of negotiation. If you were to spend 15 minutes speaking with him, you’d wish you had read one of those books because you may get hit with a pop-quiz.
Honoring All of America’s Allies
Though the war brings back bad memories, Mr. P is still able to share some details.
He was wounded in action twice, earning the Sacrifice Medal, which is Canada’s equivalent of the Purple Heart in America.
Since moving to America in 1955 the honors for his service has diminished a bit. He made it clear it was a sore subject when asked if being a Canadian veteran draws the same praise in America.
“Sometimes I’ve never felt so foreign,” he said.
Back in November, Mr. P was give the same honors any American veteran would receive as a patient of HPH Hospice.
Chaplain Scott Carley came to his home and prayed with him, thanked him for his sacrifice, and gave him pin and certificate to commemorate his service. The gesture moved Mr. P to tears.
“All I ever wanted was to feel recognized,” he said.
In total, 18 countries fought alongside America in World War II. Though most of the veterans Chapters Health System treats come from England and Canada, Mr. P and anyone else who fought alongside American soldiers can count on receiving the same treatment.
At Chapters Health System and its affiliates—Good Shepherd Hospice, Hospice of Okeechobee, HPH Hospice and LifePath Hospice, every day is devoted to educating our patients and keeping them in the place they call home. We are dedicated to ensuring that patients, young and old alike, and their families are able to make educated decisions about important healthcare matters. For more information, please call our helpful Chapters Health team at 1.866.204.8611 or send an email to info@chaptershealth.org.
Pat Carragher, Media Relations Coordinator for Chapters Health System, coordinates external communications for the not-for-profit organization.
Veteran Volunteers Needed
More than 25 percent of all hospice patients are veterans. At the hospices of Chapters Health, volunteers who are veterans are matched with patients who also have a military history. Our program is designed to offer support to veteran patients from someone who can relate more closely to their experiences. Volunteers receive ongoing training and support specifically related to veterans’ end-of-life-issues.
For more information about our openings, click over to our volunteer opportunities page, or for upcoming volunteer training sessions visit our Calendar page.
To become a Chapters Health volunteer, simply complete the online volunteer application and a Chapters Health volunteer coordinator will contact you. For more information, contact Volunteer Services at 863.551.3943 in Polk, Highlands or Hardee counties for Good Shepherd Hospice; or 727.816.3647 in Pasco, Hernando or Citrus counties for HPH Hospice; or 813.871.8237 in Hillsborough County for LifePath Hospice.



 About Phoebe Ochman
About Phoebe Ochman



 At this point in our conversation I’m thinking to myself, “Wow what hasn’t this guy done?”
At this point in our conversation I’m thinking to myself, “Wow what hasn’t this guy done?” Once a decision is made to start bullet journaling, it is fairly easy to begin. A bullet journal can be simple and minimalistic or as detailed and elaborate as you want. It is yours to make work best for your needs. You can use your bullet journal to keep track of:
Once a decision is made to start bullet journaling, it is fairly easy to begin. A bullet journal can be simple and minimalistic or as detailed and elaborate as you want. It is yours to make work best for your needs. You can use your bullet journal to keep track of: For the older adults eating vegetables, especially leafy greens and plenty of berries, the Rush group learned their brains were as sharp as those more than seven years younger.
For the older adults eating vegetables, especially leafy greens and plenty of berries, the Rush group learned their brains were as sharp as those more than seven years younger. For those individuals diagnosed with dementia,
For those individuals diagnosed with dementia,  “I didn’t realize how many resources we had available to us,” Stephen said. “LifePath Hospice has just been so on top of everything.”
“I didn’t realize how many resources we had available to us,” Stephen said. “LifePath Hospice has just been so on top of everything.”